Understanding Cow’s Milk Allergy
Cow's milk allergy (CMA) is the most common food allergy in babies and children, affecting about 2% of babies, but is uncommon in adults. Cow’s milk allergy is an immune reaction to one or more proteins in cow’s milk.
Cow’s milk allergy is different from most other food allergies because the immune reaction can involve IgE antibodies and/or other immune cells. Almost all other food allergies involve IgE antibodies only.
The symptoms of non-IgE milk allergy look different than most food allergy symptoms (see below). Babies are much more likely to outgrow non-IgE milk allergy, and non-IgE milk allergy is less likely to predict eczema and asthma (eczema and asthma are both IgE antibody related diseases).
Cow’s milk allergy is often the first food allergy discovered (as early as a couple days old) because infant formula is made from cow’s milk. Exclusively breastfed or formula-fed babies are not eating other food proteins. Learn more about breastfeeding and food allergies.
Components of Cow’s Milk Allergy
Cow's milk contains two major proteins, casein and whey. Whey proteins come in alpha-lactalbumin (ALA) and beta-lactoglobulin (BLG) forms. So a baby with an IgE mediated cow’s milk allergy can have antibodies for one or all three proteins.
Casein can come in two forms - A1 and A2. Most milk in the United States is type A1, but more A2 milks are showing up in the fridge because many people who cannot tolerate A1 milk can tolerate A2 milk.
Cooking, boiling, and baking milk breaks down most of the whey proteins, particularly BLG. About 70% babies and children can tolerate baked milk. The fermentation process of making yogurt also breaks down the whey protein, so some people with non-IgE mediated cow’s milk allergy can safely eat yogurt. People with IgE mediated cow’s milk allergy typically cannot have any yogurt.

Shop Daily Mix One-Month Supply
What Does Cow’s Milk Allergy Look Like
If a cow’s milk allergy involves IgE antibodies, the reaction will begin within minutes of drinking milk. The symptoms will look like a typical food allergy reaction with hives and vomiting / diarrhea in babies, and wheezing, runny nose and coughs in older children. Breathing in milk proteins can cause breathing reactions, and skin contact will usually cause redness and hives.
If a cow’s milk allergy involves other antibodies, parents are more likely to see persistent eczema, reflux, excessive spit-up, feeding issues, vomiting, belly pain, colic, failure to thrive, weight loss, and constipation. Non-IgE reactions often happen hours later, and the symptoms may last for multiple days.
If your baby is vomiting a lot or has daily runny poops, they should be evaluated for food protein-induced enterocolitis syndrome (FPIES). Bloody or mucousy poops need immediate attention and may be food protein-induced proctocolitis.
Non-IgE allergies to cow’s milk can also cause food protein-induced enteropathy (FPE) which results in failure to gain weight or Heiner syndrome which involves a persistent cough, recurring fever, ear infections, etc.
Always talk to your doctor about an elimination diet if you see any of these issues. Do not allow anyone to tell you colic is normal!
Testing for Cow’s Milk Allergy
In babies who are showing signs and symptoms of a cow’s milk allergy, a first step is often an elimination diet (mom eliminates if breastfeeding) to see if the baby's symptoms clear up. Avoidance of cow’s milk for about 5 days is usually enough to tell if your child has an allergy, but it will not tell you what kind of allergy it is.
Blood, or specific IgE testing for cow’s milk allergy can help to know if the allergy is IgE mediated. Testing can be performed for each cow’s milk protein such as casein, ALA, or BLG. Even the component testing won’t tell you if your child can tolerate baked milk. The only true test is an oral food challenge.
Cow’s Milk Allergy vs Lactose intolerance
Cow’s milk allergy is a reaction that involves the immune system, and you will see the typical signs of an allergic reaction. Even a tiny amount of milk can cause the reaction.
Lactose intolerance is a failure of the gut cells to digest and absorb the sugar lactose which is found in milk. Some people’s guts do not produce the chemical lactase, which is needed to digest lactose. Undigested lactose makes it to the colon where it is converted to hydrogen gas by the colon bacteria. This fermentation is what causes the pain, bloating, and, well, gassiness of lactose intolerance. People with lactose intolerance can eat lactose-free milk like yogurt where the live bacteria eat up the lactose sugars.
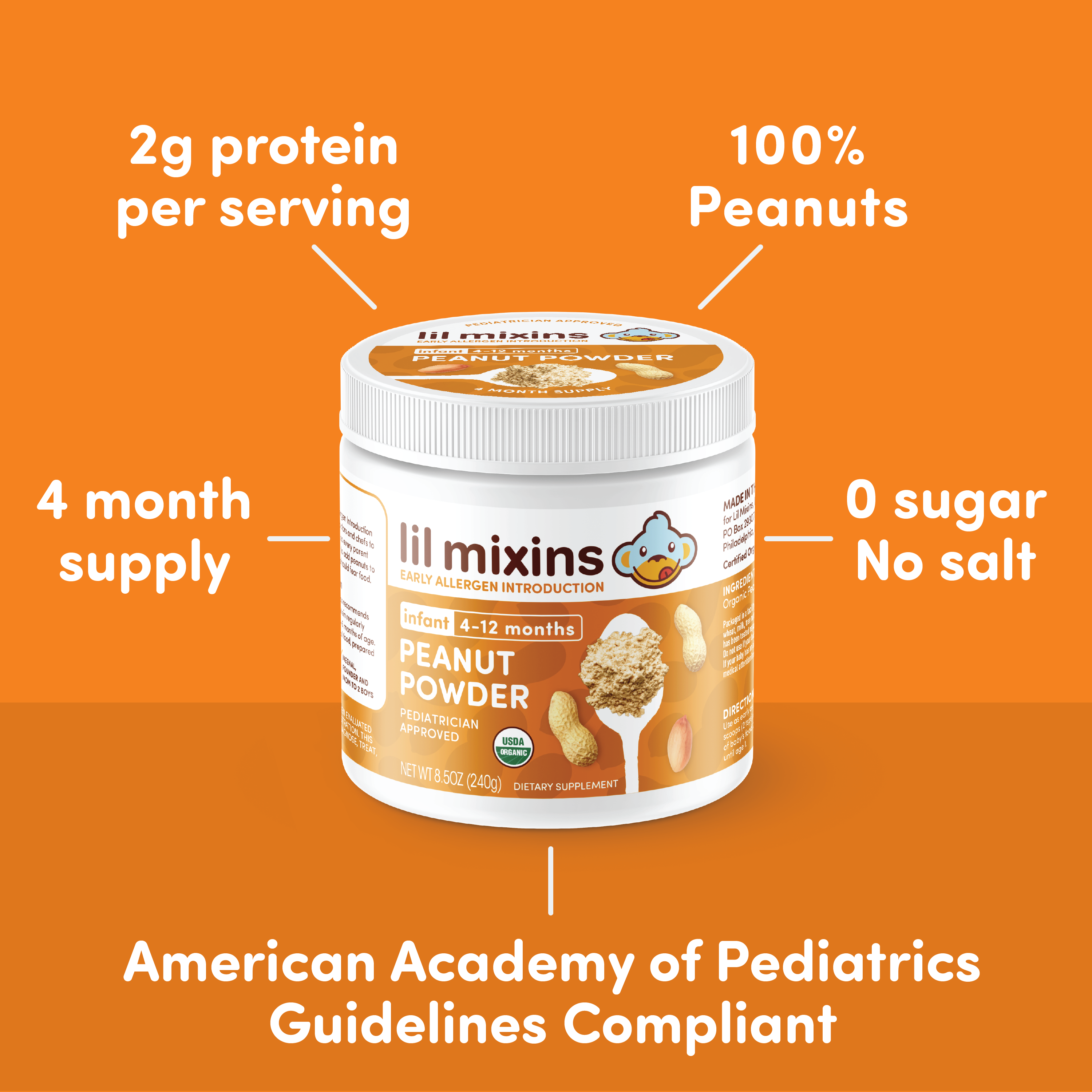
Shop Peanut Mixin 4-Month Supply
Outgrowing a Cow’s Milk Allergy
The good news is that most children outgrow cow’s milk allergy, especially if it is non-IgE mediated. Even three quarters of children with IgE mediated allergy eventually outgrow it! Being able to eat baked milk, and regularly eating it seems to increase the chance of outgrowing a cow’s milk allergy. As with all allergies, kids with fewer IgE antibodies and fewer other allergic diseases are more likely to outgrow cow’s milk allergy.